|
These are definitely uncertain circumstances and uncertain times in the world at large, and the world of Play Therapy. When our clients are at their most vulnerable, we have decisions to make about the best ways for us to show up for our client’s and provide this service. AND these decisions are much more complicated than a therapist shifting their practice to virtual sessions under almost any other circumstances. Conversations with clients this week have been on a continuum of concern to sheer panic, but one common theme of uncertainty united them all. Change of routine, as schools in Minnesota have closed, and much fear about underlying health conditions for children themselves, siblings, family members, and friends that may place them at risk should they be infected with COIVD-19. Uncertainty of how long this will last, disappointment about cancelled events that young people have worked SO HARD for, such as concerts, sports seasons, and class trips, and frustration with not being able to see friends. There has also been much confusion and difficulty understanding WHY things can’t be normal. In all this time of uncertainty the consistency therapy provides can be a safe harbor for our clients to begin to unravel all of these complex emotions. This week I have reflected significantly on what my clinical recommendations would be for clients as I transition my practice fully virtual in an attempt to do my part for both myself and the families with whom I work with to social distance. The great news is that all clients have autonomy over their mental health care at all times. I can offer what I believe to be the best recommendations for their mental health treatment, and they have the option to take it or leave it. I in no way want to spread fear, as there is plenty of fear and panic in the world right now. However, I do not want to be ignorant as I am watching the COVID-19 pandemic unfold across the world. I think we need to get real and honest with ourselves and our clients. This is not a one or two week break. Schools are talking about being out of session until the end of the year. And if I am thinking about the impact of this time frame on someone’s mental health services, this is a significant shift in their therapeutic care. As I sat and thought about each of my client’s mental health needs, I reflected on the question – do I believe that our current pace of therapy is medically necessary? How would I (for any other reason) respond with therapeutic recommendations for a client that wanted to take a 2-3 month break from therapy? What would be my ethical duties to inform them of what that might do to their mental health? For most of our clients, we would likely say that this amount of time without service would be detrimental to their mental health and progress. With the reality that some states have begun to require residents to “shelter in place” as well as social distancing recommendations, it is realistic to think that most clinics will be faced with the decision – virtual vs. no service. In this decision I look to the American Counseling Association Code of Ethics which states, “Counselors assist in making appropriate arrangements for the continuation of treatment, when necessary, during interruptions such as vacations, illness and following termination.” Read more about therapy interruptions and our ethical duties here. Considering this information, for those that are not able to provide services virtually there needs to be a referral for clients to continue care elsewhere should you not be able to provide that service or significant resources put in place and a plan to receive services should they decide they want to re-engage in therapy and you are not able. If I think to my nine week maternity leave – SO MUCH planning and preparation went in to making sure each client was connected with another therapist for the interim or for those who elected not to continue a specific plan was made and a referral was given should they need to see a therapist during that time as I was not able to provide them therapeutic care. I strongly believe as a Play Therapy community, our leaders should be those who have expertise in this work and who have been doing it in the field with children and adolescents. We can look to therapists such as Dr. Tillman, PhD of the Family Institute out of North Dakota who has been offering virtual Play Therapy services for 6 years to serve the remote families on her caseload that have difficulty with access to in office appointments and Lisa Dion, LPC of the Synergetic Play Therapy Institute who talks about her experience with virtual Play Therapy here and here and so many others that are offering trainings, materials, and adaptations. For those of you still taking a breath, getting clear, and deciding what is right for you, your clients, and your practice – that’s OK too! If you are not regulated and in your window of tolerance it’s ethically best to take a step back and get clear about the pros and cons of each as well as develop an action plan. So - here is the 1,000 foot view of what might go into this process as you make these decisions. Get clear on the rules: There are so many invested parties when you think about shifting your practice to Telemedcine/Telemental health. The first is what does your specific state laws and licensing board say about what is needed to provide this service? State law varies state to state for what is required to deliver this service. AND licensing boards may vary across licenses within the same state! For my state of Minnesota as a Licensed Professional Clinical Counselor my board has different requirements for where a client needs to be in the present moment (“feet on the ground”) versus other boards. Next is your malpractice insurance. I carry my own malpractice insurance in private practice and the feedback I received was that I was covered whatever medium I choose to provide therapy. However, this is policy and insurance company specific! Next consult your ethics code. See about how I went through my ethical decision-making tree HERE! Lastly the client’s insurance company may also have specific requirements as well, so even if you are able to provide this service according to your state law, licensure board, and malpractice insurance your client’s insurance may not allow you to provider therapeutic services in this way. Get Trained! With anything new according to our ethics codes, additional training and education is required. It is an amazing time to see the mental health community band together and offer FREE training of how to ethically and appropriate transition sessions to telemedicine. Some have CE Credit, like this PESI training below, and some are for your education as a therapist without CE credit. PESI is offering their course “Telehealth for Mental Health Professionals: 2-Day Distance Therapy Training” FREE with the code TELEFREE at checkout! (usually $439.99). Still feeling unsure? Think about getting supervision or consultation around this topic with someone who has provided this type of service! Get Prepared After your training you will likely know what resources you will need to pull together to ethically begin to provide this service to clients. I write about more about what you need HERE and offer a free-mini course about how to get started. Person Centered Tech also offers AMAZING resources HERE including forms, a free training video, and preparation checklists. Give Informed Consent Giving clients informed consent should be more than handing them a packet or sending them a form and asking them to sign at the end. The informed consent, especially during the COVOID-19 pandemic, allows clients and their families to make decisions that are best for them. My free course has the Telemedicine Informed Consent I use with clients. Collaborate with Clients I talk HERE about how to have an Orientation Session with clients after they transition from in office to Telemedicine. I include two free downloads of handouts to send to parents to help orient them to the technology and virtual platform. I also talk about how to brainstorm about how to make these sessions, within the home, safe, ethical, and confidential. Modify I strongly believe that providing therapy on a virtual platform for Telemedicine or Tele-Play is a modification of an existing skill set. I have provided therapy services across a wide range of settings including in office, schools, homes, and juvenile detention centers. Each of these settings needed special adaptations for me to ethically, privately, and competently provide services as a therapist. Providing services virtually is another setting with its own unique set of challenges. Much like in home we need to think about how to create a safe, private, and confidential space in their home. The additional setting challenge includes how do you provide safety should a situation arise that the child is out of their window of tolerance and you are not able to use skills to regulate or they are a danger to themselves or others. These structures should be built into every safety plan created with clients, may vary from client to client, but generally includes close and easy access to a parent and training the parent to engage in a safe ethical way when needed. With these modification bumpers in place the heart of the work remains the same. The relationship you have with the client, the core interventions, and your theory. Are you thinking about transitioning clients in your practice OR are you in the middle and finding it hard to become clear with all the moving pieces? Grab this spreadsheet to ensure you have all the proper forms and communications in place with your clients. Let's Connect - click here to join my email list!
3 Comments
With all the changes happening around the country and the mental health world, the therapy field has had to rapidly transition from in office sessions to Telemental Health sessions. I wrote HERE about my scripts to orient children and their families to Telemental Health sessions BUT what now? What about from the time you say your last good by to clients in the office (for now) and before you turn on the camera for your first appointment? I want to be really honest here – this feels so different than when I offered this service and began the journey of Telemental Health a little under a year ago. There is a general anxiety around the conditions for transitioning AND we haven’t been preparing for weeks and months for the transition as I did with my in office clients when transitioning my practice from the twin cities area of Minnesota to Duluth. First and foremost – it is our job to be prepared, have a plan, and be able to talk about options with clients. My scripts spell out how I’ve been talking about the transition with parents. However, in this case because there is SO MUCH anxiety and quick decision making I know that everyone, including me, is not fully in their prefrontal cortex and some (if not most) of the information gets lost. So I put together two cheat sheets for parents to read and reflect on before our first session. You can find them both for free to use and edit to your heart’s desire HERE! The fist sheet simply orients to WHY online, what it might be like, and what are the specific nitty gritty things you need for a good call. These include a fast internet speed, closing out all other programs, having headphones, how to get on the appointment and instructions for accessing the platform. The second sheet was a quick takeaway of strategies for HOW to set things up. In my past transitions these again were things we talked about and touched on for weeks if not months as our in person sessions were winding down. The second handout includes how to find a good room, how to ensure confidentiality (which was the biggest question my young people had) including not having a sibling bust in the room during their time, safety procedures, and so on! Another bonus of handouts is it sends the message to clients that you really have your stuff together. That you have thought this through and have a plan in place! One of my favorite quotes is "trauma is chaos, structure is healing" and this my friends, is the structure! Now, before you turn on the camera to start the session I have found that if you are shifting to directive techniques, or even if that was your camp before, there needs to be prep before the session. You need to think about what specific activity you will be doing with clients and think through what supplies they may need. My post of Telemental Health and Children: 20 Free and Minimal Supply Activities takes you through some ideas with a specific supply list for each. If you use any of these you can copy and paste from the post. Okay – so you have emailed the parent about what supplies they need, ensured they actually have these supplies, and you have the supplies you need on your end. As you turn on the camera you need to have an Orientation Session that includes the following: Confirming address and best number to reach the client: This is one of those safety procedures to ensure that you can have contact with a parent at all times. Make sure that the number you have listed in their chart is the number you can actually reach them at and set the stage that they will be available to enter the room at any time via this number. ALSO make sure the address you have on file is actually their address. How many times have you had clients move and in the chaos of it all forget to update their address with you? Additionally many families I work with reside in two homes - make sure you have the correct address for the correct parent or guardian! I have begun to create cards for each child (on bright pink index cards of course) of address, best number to reach them, and number of local police department. This as well as my cell phone (which they have the number to be able to contact me if they need) sits out by the computer during the session. Assessment of technical aspects: Process if there was any difficulty accessing the technology. Address any questions they may have. Go over technology safeguards. Mine is that if it glitches for over 2 minutes I will call them while we attempt to re-logon. With some children it might be immediately if it goes off you call a parent for assistance. Explore what this might mean for the specific family and child. Assessment of space selected: Together process what went into picking the space, if others can hear, how the parent will keep siblings out of the room (if applicable), and if there needs to be any additional safeguards such as a radio outside or sound machine. Assessment of parental involvement: For each child assess what the set-up will be with how active and involved the parent is. Will the parent set up the technology and have the child take the lead from there? Do you have a child where the parent will need to be an active member in the session OR will they need to be present in the room but not involved in the session? Each family will be different so this discussion will be helpful to determine what fits for each specific child. Assessment of session structure: This has been the question that comes up most with families – “will it be the same”? I am attempting to keep my sessions as similar as possible to in office work. For me that means checking in at the beginning (with or without the child depending on the client) and the child having the majority of the session to themselves BUT I am now adding a “check out” at the end. I usually do a casual goodbye in the waiting room, so for the young people I work with that will be in the session by themselves for a period of time I have developed a procedure to “check out” with the parent at the end – just a friendly wave that we are done! For teens this may be less important or necessary. For some clients a new structure might be transitioning from nondirective sessions to directive sessions. Orient the client to these any any other changes with the structure of their time with you! SO as I roll this out to families my motto with parents and families has been “assess, pivot, assess, pivot, assess, pivot”! Meaning that each session we will spend a small amount of time assessing how things are going and pivoting if necessary. What additional tips do you have for your first session? Drop them in the comments below! Let's Connect - click here to join my email list!
As the Coronavirus pandemic grows, many in the mental health field are faced with the real possibility of some or all appointments needing to move to Telemental Health services. This hit home in my practice this week as I now have my first child clients going into a self imposed “social distancing”, which is a conscious effort to reduce close contact between people. Schools, sporting events, and large gatherings are being cancelled across the United States, even the training I was waiting all year to see. Ahhh! So many feelings are coming up for us as therapists and the families we serve. It hit home even further today as all schools will be closed in Minnesota effective Wednesday. There are many in the mental health community who serve young children who are feeling helpless and hopeless for how to develop a plan to move forward. For the younger children I see, I am primarily a Child Centered Play Therapist – so nondirective. Over the past weeks I have been faced with a choice of how to move forward as I radically accept the Coronavirus, its spread, and its impact on daily life. I have also been SO touched and moved with the way the Play Therapy community has come together to support one another, including the development of the “Tele-PLAY Therapy Resources and Support” facebook group. If we dive into the fears that some therapists may have about just what might happen during these appointments that hold therapists back, hopefully we can become clearer on the answers of how to move forward. At the beginning of my Telemental Health journey I began brainstorming what were the potential risks with children specifically. These were sessions where their parent or a guardian would be at the residence the entire duration of the session. Okay – so here is what my list looked like. What if they run out of the room? What if they turn off the camera/program? What if they take the device and go on other programs? What if they don’t listen to what I say? When I sat down to think about these things, I actually realized that I feel safer providing Telemental Health to children than adults. Children will always have an adult I can connect with if they are having difficulties. I developed a procedure to have parents accessible by phone for the duration of the appointment and I have easy access to their phone number and my phone. This means, if any of these things happened, a parent would quite quickly be able to engage in the room. I also reflected that some of these things happen within office too as part of the therapy process and most of us have a theory or procedures in place with how we handle clients not complying with limits or boundaries. Also, consider if limits may need to be set sooner to ensure the child stays in the window of tolerance to be able to engage with you. Lastly, brainstorm for your practice what will happen if they child is not able to comply with limits? Will the session be over? Will the parent join for the remainder of the session? Now, on to my next set of worries. What if they become distressed and begin to have a meltdown? What if they are throwing things or in physical danger? Again, I came back to quick and easy access for parents and extra safety precautions that I clearly review policies with parents that if there is a true crisis I will call 911 and will have their address easily accessible at all times. When I really thought about it hard, this would be no different than a child playing alone in their room for 30 or 40 minutes. AND what I know is that children get dysregulated at home all the darn time. How often do we hear about fights with siblings or a client completely melting down over losing a video game? Parents are present for those situations and have been the ones “in the trenches” responding to these episodes for the child’s entire life. You will want to have extra brainstorming and policies with parents around how they might handle this should it arise – which may look different for each client. Other potential difficulties I brainstormed was the child that did not want to engage in a virtual session – the child that left the room, had a tantrum when the appointment started, got bored and tuned you out - you get the picture. When I thought about it many children are familiar with a video chat platform like Facetime of Skype so this likely won’t be their first video chat. BUT I also know this could be very anxiety producing for children. I then considered what “buffet of options” I could provide to support families with. Would this be a child where parent and child sessions would be more beneficial? Would this be a client who I would meet with the parent only and potentially reduce session frequency? Would the child be receptive to certain activities over others? Then my mind wandered to age – what if they are too young? I then began thinking about what age would I ethically consider young enough to be unsupervised in a room for 30 minutes? Yes, as an adult I would be watching virtually what was happening in the room so they wouldn’t be truly alone, but I wouldn’t be able to physically intervene. My personal style is to check in together with parents and children, so 30 minutes is the minimum that I typically like to have with children alone. I also considered the emotional and maturity age and how this may be different with different clients. Another solution I thought was for children who may not be able to handle 30-40 minutes, could I alter sessions and do a 90832 session OR have sessions that were family focused with the parent in the room? Another idea I had was to have the parent physically present in the room, but not in the session. Maybe the parent has earphones in and are catching up on their favorite TV show? Lastly I came up with questions and worries about the technology. What if they don’t know how to work the program? Then I realized that most children are more proficient in technology than adults. I also know that a parent setting up the technology and being able to call the parent to assist should connection be lost and a re-set is needed would be something that would be a potential solution. As I sat down with all of this information and consulted the ACA Ethical Decision Making model I found nearly ALL of the foundational ethical principles applied. The first was Autonomy – providing my clients and their parents the right to make a choice about how they wanted to proceed with their mental health services. Next up – non-maleficence. How in this dilemma was I going to ensure that I was not causing harm to my clients? I weighed the pros and cons of no services (for weeks or months) OR an altered format (more directive, shorter appointments, etc.) via Telemental Health. How could I avoid client abandonment? Then comes beneficence – what will be the decision that will be in the best interest of the client? Again, I weighed the benefits of providing this service as a new format of therapy (virtual and directive) versus no services. Lastly is fidelity “honoring commitments and keeping promises, including fulfilling one’s responsibilities of trust in professional relationships.” How does this crisis fit with my commitment to clients? After considering these principles and weighing pros and cons of each, consulting my ethics code, state laws, board requirements, and insurance company requirements I decided the best course of action was to prepare to provide this service as an option and choice to families should they ask about it or be unable to engage in therapy due to circumstances such as quarantine. I decided I needed to continue to offer to provide mental health services as a consistent factor in their life as well as keep the connection and relationship in uncertian times. Interested in more about starting Telemental Health Services with children and adolescents? Take my free E-course HERE. It includes more comprehensive outline of Telemental Health services, a resource list, a “Cheat Sheet” to orient clients to Telmental Health and an informed consent template. Now, before we get into the good bits of what this might look like, I wanted to take some more time to talk about how we roll this out to our families. If I’m being really honest, how comfortable families feel with this therapy starts with US. If they inquire about it and we are anxious, frantic, or panicked OR we don’t even have a plan, families are definitely going to feel uneasy about getting their child’s mental health needs met in this way. I can tell you that it felt amazing to tell my clients this week “yes we can definitely set that up. Our clinic has been working on a plan to help support clients that need or would prefer to have virtual appointments. Here is a sheet that will help guide you though the login process and we can sign an additional informed consent and discuss the specific risks and limitations of Telemental Health”. These families – they were relieved that I had already been thinking about this and had measures in place to support the way they felt most comfortable having sessions. When I rolled this out to the young people I was working with it sounded a little like this “There are some really big things going on in our country right now. What do you think I am talking about? [prompting children to engage in their own language to describe the pandemic]. Yes! [paraphrase child’s response]. Now, I know your family is making some decisions with how to keep you and your family safe. What do you know about that? [prompt dialogue in the child’s own language about the changes]. Yes! [paraphrase child’s response]. There may be a lot of changes in your life because of this like not getting to see your friends for a bit or go to the activities you like, but the good news is we will still get to meet virtually! Have you ever had a time that you talked to someone over video on the phone or the computer? [prompt a dialogue about their experiences with video chatting platforms]. Now for us, our sessions might look a little bit different. I know most of the time you get to be in charge in here and decide what to do. When we meet virtually I will have an activity or project set up for us and will let your parents know exactly what you need to have for our time together. Now, what questions do you have? [prompt discussion about fears, worries, or wonders].” Lastly some tips of how to prepare and orient these sessions. The most frequent question I have is how to keep the sessions private. Brainstorm with parents what room of the house is the most beneficial for privacy and utility. Discuss the option of playing a radio outside of the room for extra confidentiality, especially if siblings will be home. Discuss how parents can ensure that siblings maintain good boundaries. Have them practice before hand of where to place the device. Email parents a “supply list” of what they need to have on hand for the sessions before the session. Evaluate the need for an altered structure. I usually say a casual goodbye to parents in the lobby as we transition but evaluate if there may be a need for the parent to come on camera and officially end the session. Oh and lastly – I made a commitment to my clients that I would tally how many virtual sessions we had together and they would get to pick that many treasures from my treasure box when we resumed in person sessions. I definitely didn’t think it was fair to withhold the treasure! Okay – now to the activities! I actually had so much fun putting this together and the ideas just kept flowing! I created this list with the minimum amount of supplies necessary that all families likely have on hand at home! 20 Free, Low Prep, and Minimal Supply Activities for Telmental Health With Children:
Here are some additional things to consider – all online programs you are asking clients to use should have informed consent from a parent and clear communication about why you would like the child to access such a program. You should never engage in the chat feature of any online shared program (if applicable) as it is not HIPAA compliant. Lastly – if there are no markers, colored pencils, or crayons to be found in the home you can have the child draw different patterns to symbolize different aspects and create a “key” of sorts to code it all out. I hope this gets your wheels turning about free and low prep activities that you could modify to work well with Telemental Health child clients! We are creative. We are play therapists. WE CAN DO THIS! Interested in more training? Check out my Cognitive Behavioral Play: Low Cost and Preparation Training for Telemedicine and Tele-Play that is approved for 3.25 APT Non-Contact hours by Meehan Mental Health Services (APT Approved Provider 19-580). Drop a comment with your favorite free, low cost, low prep activities that you are thinking about using for Telemental Health with kids! Let's Connect - click here to join my email list!
In light of the recent coronavirus there has been so much talk in the therapy world about using Telemental Health/Telemedicine as a back up plan should clients become ill or quarantined. I started my Telemedicine journey a little over a year ago as I began my plan to relocate my practice across the state from the twin cities metro area of Minnesota aallll the way “up north” to Duluth. I wanted to give my clients more options for what might be right for them as I transitioned. Some clients used it as a way to bridge the gap between in person sessions and when their new therapist had openings for service. Other clients found that it was their ideal way to engage and receive therapy – so they stated on permanently as Telemedicine clients. Now there are a TON of terms for what we know basically as the therapist being at one location and providing services to clients at a second location – Telemedicine, Telemental Health, E-therapy, virtual therapy, online therapy – wheew! I have chosen to call what I do Telemedicine, as it is the larger umbrella of services that Telemental Health falls under AND it is what my state statute uses to describe this service. After diving into to Telemedicine, I have to let you know...I LOVE it! I often find that clients can be more relaxed in their home and it can be easier to get into the tough stuff more quickly as clients are surrounded by an environment that is known and comfortable to them. I also find that it is super helpful for homework and prompts. There is no more barriers such as leaving a project in their bedroom, or if there is something I am wanting them to do (like put a quote on their mirror or post-it on their door) they can do it in real time! As I am hearing all this conversation about Telemental Health I honestly started to become a bit anxious. As a therapist who spent over three months gearing up, researching, training, helping to develop policies and procedures, and helping clients understand exactly what this service was – I was hoping that therapists understood it was SO MUCH MORE than finding a HIPAA complaint online platform, turning on the camera, and having a session. Especially since every now and then you hear a comment like “I can use Skype right?” So here’s the tip of the iceberg of what you will need to get a Telemental Health practice up and running:
Whoa. Now, if you are like YES! I know exactly what you are talking about and I am all covered for these things – that is amazing! You are so ready! If this list freaks you out – you probably have some work to do to get your practice ready. This is why I developed a FREE e-course about getting your Telemedicine practice up and running including a FREE informed consent template, Telemedicine Resource List (complete with a comparisons of platforms that are HIPAA compliant), and a handout I use to explain and orient clients to Telemedicine services. Does this some like something you need? Take me to the course! Also check out the Lessons From The Playroom podcast episode 32 to get you inspired for how to use play therapy in your work with Telemedicine! Lastly, this free mini e-course is for informational purposes only and does not offer any continuing education credit. It is solely my opinion, which I have gathered through trainings and real world experience providing Telemedicine services. It is to help you understand if Telemedicine could be right for your practice and some of the things that are necessary to have in place before you start. Imagine curling up with a cup of coffee to chat with one of your friends to see if Telemental Health services are right for you - and that friend just so happens to have a TON of details, templates, and resources for how to get your Telemental Health practice up and running! Let's Connect - click here to join my email list!
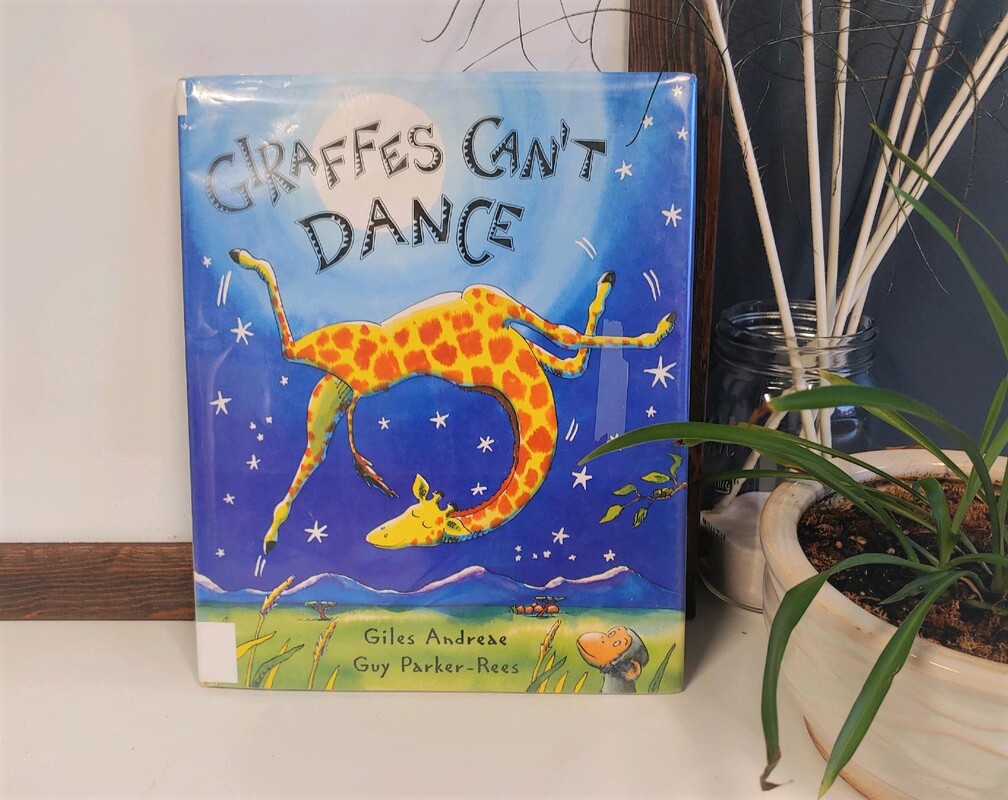
“Giraffes can’t dance you silly fool, oh Gerald you’re so weird.” I literally have this book memorized. I could recite it in my sleep – no joke. Not only because I use it all the dang time in my therapy sessions, but my son also happens to love it too! AND what’s not to like – an underdog truly coming into his own to become the BEST dancer anyone in the jungle has ever seen! Ok, let me back up a minute. You all know how much I love bibliotherapy, and if you haven’t read Giraffes Can’t Dance scoot yourself to the nearest bookstore, pop it in your Amazon cart, or to be honest you can see it right now on youtube! In this book, Gerald the giraffe learns that animals in the jungle can be unkind and downright mean, but with the help of a cricket, confident thinking, and his own special song he can do anything he puts his mind to - including dance! This book has it all – self-esteem, bullying, growth mindset, self-talk, connection and support. It is also ah-mazing for Cognitive Behavioral Play Therapy. There are so many opportunities to go through the cognitive triangle and connect thoughts, feelings, and actions. It is also filled with regulation skills and highlights Gerald’s self-talk. You can clearly see the pattern when Gerald makes statements that he is “such a clot” and how they connect with him feeling sad, giving up, and going home. Giraffes Can’t Dance also highlights the importance of helpers – a small cricket steps in and serves Gerald some serious wisdom allowing him to find his rhythm and a song that is just for him. You can see the shift in Gerald’s mood as he exclaims “I AM DANCING”! He is also incredibly gracious and doesn’t even dish out as much as an “I told you so” to any of the jungle animals – he just finishes with a bow. Gerald is one class act. My favorite companion activities for this book include a “Find Your Song” activity. You have young people identify a song that is just for them – the music they move through life to. You can play the song in session, notice what feelings and thoughts come up, or have them focus on a specific powerful self-statement. This book is also a great tool for EMDR as it helps identify feelings, thoughts, and cognitions. You can get curious about where Gerald may feel sensations in his body and what pictures may be going through his head as well as giving Gerald a Subjective Units of Distress rating. This primes young people to head into phase 3 of EMDR desensitization and reprocessing and gives them language and examples when asking about TICES. You can also use the “Find Your Song” activity if you are trained in EMDR with slow bilateral stimulation for the development of a resource. I have also developed a worksheet pack that I use with young people including a Giraffes CAN Dance growth mindset worksheet that helps young people evaluate things they thought they couldn’t do but actually could as well as things they can’t do YET! For young people who feel isolated or alone you can grab the “Who Are Your Crickets” worksheet to help them identify their community and team. I have also used this for big transitions in life such as from elementary school to middle school or out of intensive outpatient treatment into a less restrictive setting. The last worksheet in the packet, "Who Are You A Cricket To" can be used for social skills. You can help young people identify how they show up for others and encourage others. You can grab your free downloadable worksheet pack HERE! This is such an amazing book that I have used it different ways and different times with the same client. Maybe one time to talk about confidence and finding a client’s song and again for a transition time when she needed to get clear about who was on her team. I know this book is so dynamic – drop a comment with other ways you have used this book in your practice! PS - why YES that is a giant piece of tape on my book! This is one of the original books I purchased as a play therapist with a tiny budget. It came from a little website called half.com where I was used to buying some of my college text books. This copy is from the New York Library! Interested in learning more about how to use Bibliotherapy in your Play Therapy Practice? Check out this training HERE! Let's Connect - click here to join my email list! *This post contains affiliate links, so I may earn a small commission when you make a purchase through the links on this site. The best news? It doesn’t cost you a penny! Thanks for supporting The Playful Therapist Blog by shopping my favorite playroom gear and accessories! |
Hi, there!I'm Ann Meehan, an LPCC, Loading... Archives
July 2024
Categories
All
|
Privacy Policies | Terms of Use | Disclaimer
Contact
[email protected] | Copyright Meehan Mental Health Services 2022
Contact
[email protected] | Copyright Meehan Mental Health Services 2022